Cardiomyopathy
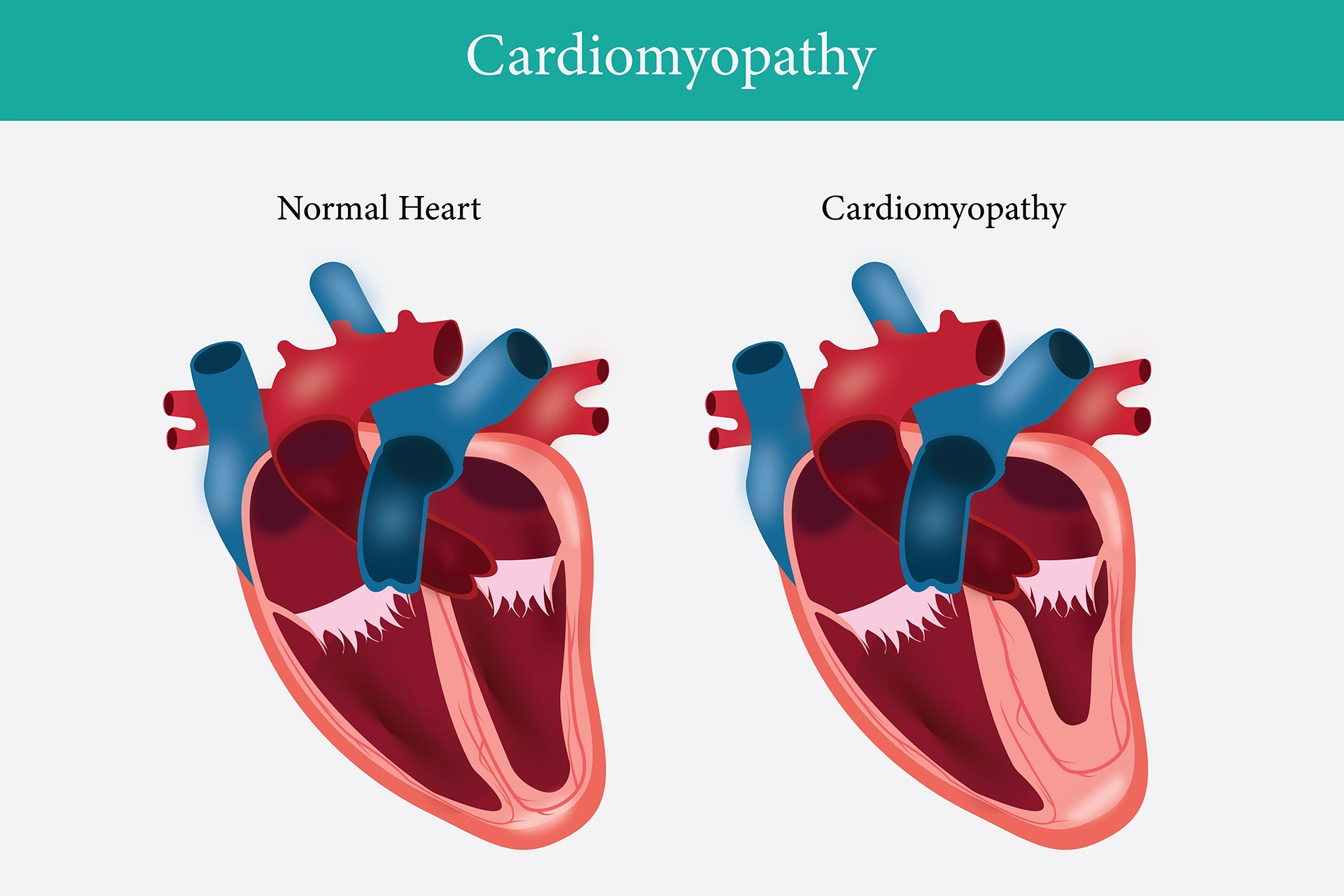
Cardiomyopathy is a disease that affects the heart muscle, making it harder for the heart to pump blood efficiently. Over time, it can lead to heart failure and other serious complications. Some forms of cardiomyopathy are inherited, while others develop due to underlying health conditions or lifestyle factors.
There are different types of cardiomyopathy, each with varying causes and treatments. Some cases require medications, lifestyle modifications, or surgically implanted devices, while severe cases may require a heart transplant. Early diagnosis and proper management can help improve outcomes and quality of life.
Types of Cardiomyopathy
Cardiomyopathy is classified into several types based on how the heart muscle is affected:
- Dilated Cardiomyopathy (DCM) – The heart’s chambers enlarge, causing weakened contractions and reduced blood flow. This is the most common type and often leads to heart failure.
- Hypertrophic Cardiomyopathy (HCM) – The heart muscle thickens abnormally, making it harder for the heart to pump blood effectively. This condition is often inherited.
- Restrictive Cardiomyopathy (RCM) – The heart muscle becomes stiff and less elastic, restricting normal filling of the heart chambers. It is more common in older adults.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) – A rare genetic condition where the heart muscle is replaced by fat or scar tissue, increasing the risk of arrhythmias and sudden cardiac arrest.
- Unclassified Cardiomyopathy – Other forms that do not fit into the above categories.
Symptoms of Cardiomyopathy
Many people with cardiomyopathy do not experience symptoms in the early stages. As the condition worsens, symptoms may include:
- Shortness of breath (especially during physical activity or while lying down)
- Chest pain, often after exercise or heavy meals
- Irregular heartbeats (palpitations)
- Fatigue and weakness
- Swelling in the legs, ankles, feet, or stomach
- Dizziness or fainting
- Persistent cough (especially when lying down)
Symptoms may develop gradually or worsen suddenly. If you experience severe difficulty breathing or chest pain lasting more than a few minutes, seek emergency medical attention immediately.
Causes of Cardiomyopathy
The exact cause of cardiomyopathy is often unknown. However, it may result from inherited genetic conditions or develop due to external factors.
Inherited Causes (Genetic Cardiomyopathy)
- Family history of cardiomyopathy or sudden cardiac arrest
- Genetic mutations affecting heart muscle proteins
Acquired Causes (Secondary Cardiomyopathy)
- Long-term high blood pressure – Puts excessive strain on the heart
- Heart attack or coronary artery disease – Can weaken heart muscle
- Metabolic disorders – Diabetes, thyroid disorders, and obesity increase the risk
- Alcohol and drug use – Chronic alcohol consumption, cocaine, or amphetamines damage the heart
- Infections – Viral infections, including COVID-19, can cause heart inflammation
- Autoimmune and inflammatory diseases – Sarcoidosis, amyloidosis, or connective tissue disorders
- Chemotherapy and radiation therapy – Some cancer treatments may damage heart tissue
Risk Factors
Several factors may increase the risk of developing cardiomyopathy, including:
- Family history of heart disease
- Long-term high blood pressure
- Coronary artery disease or a history of heart attack
- Obesity, leading to increased heart workload
- Excessive alcohol consumption or substance abuse
- Certain chronic diseases, such as diabetes or thyroid disorders
- Prior use of chemotherapy or radiation therapy for cancer
Understanding these risk factors can help with early detection and preventive measures.
Complications of Cardiomyopathy
If left untreated, cardiomyopathy can lead to severe health complications, including:
- Heart failure – The heart struggles to pump enough blood to meet the body’s needs.
- Blood clots – Reduced heart efficiency may cause clots to form, increasing the risk of stroke.
- Heart valve disease – An enlarged or weakened heart may lead to improper valve function.
- Arrhythmias and sudden cardiac arrest – Irregular heart rhythms can be life-threatening.
Diagnosis
Diagnosing cardiomyopathy involves a combination of medical history, physical examination, and specialised tests, such as:
- Electrocardiogram (ECG/EKG) – Detects abnormal heart rhythms
- Echocardiogram – Uses ultrasound to visualize the heart’s structure and function
- Cardiac MRI or CT scan – Provides detailed images of the heart muscle
- Stress test – Assesses how the heart responds to exertion
- Genetic testing – Recommended for individuals with a family history of cardiomyopathy
Early detection is key to managing symptoms and preventing complications.
Treatment for Cardiomyopathy
Treatment depends on the type and severity of cardiomyopathy. It may involve medications, lifestyle modifications, or surgical interventions.
-
Medications
- Beta-blockers – Help slow heart rate and reduce strain on the heart
- ACE inhibitors – Lower blood pressure and improve heart function
- Diuretics – Reduce fluid buildup and swelling
- Antiarrhythmic drugs – Help control irregular heart rhythms
-
Lifestyle Changes
- Maintain a heart-healthy diet with low sodium and saturated fats
- Engage in regular physical activity approved by your doctor
- Manage stress levels through relaxation techniques
- Avoid alcohol, tobacco, and illegal drugs
-
Medical Procedures & Devices
- Pacemaker – Helps regulate slow or irregular heartbeats
- Implantable Cardioverter Defibrillator (ICD) – Prevents life-threatening arrhythmias
- Septal Myectomy – Surgical removal of thickened heart muscle in hypertrophic cardiomyopathy
- Heart Transplant – Considered for severe, end-stage cardiomyopathy
Prevention & Heart Health Tips
While some types of cardiomyopathy are genetic and cannot be prevented, you can lower your risk of acquired cardiomyopathy by:
- Controlling blood pressure, cholesterol, and diabetes
- Avoiding alcohol and drug use
- Staying physically active and maintaining a healthy weight
- Eating a balanced diet rich in vegetables, lean proteins, and whole grains
- Managing stress through mindfulness or relaxation techniques
Taking proactive steps can help you maintain heart health and improve your quality of life.
When to See a Doctor
If you experience persistent symptoms such as chest pain, shortness of breath, or fainting, consult a cardiologist immediately. For those with a family history of cardiomyopathy, regular check-ups and genetic screening may be beneficial.
If you suspect a cardiac emergency, call 999 or seek urgent medical assistance.
📅 Book an appointment with our heart specialists today for a comprehensive heart health assessment.